Fast Facts
Adapted from Fast Facts for Medicaid Expansion by Georgia Budget & Policy Institute
- One thing Gov. Kemp and the state legislature can do right now to protect families is to expand the Medicaid health insurance program so that more people have health coverage and can get care if they become sick without worrying about large medical bills afterward. Most states have already taken this step – it is time for Governor Kemp and our state legislature to do the right thing and expand Medicaid.
- Immediate Medicaid expansion would save lives, provide desperately needed coverage to Georgia’s most vulnerable, accelerate economic recovery and stabilize rural health systems.
Key statistics:
- In total, over 560,000 Georgians would be able to see a health provider and not worry about facing medical debt if the state expanded Medicaid.
- 408,000 low-income Georgians[1] do not qualify for Medicaid in Georgia and make too little to get financial help to buy private insurance at healthcare.gov. These Georgians have incomes below the poverty line (less than $12,567 a year for an individual or $21,429 a year for a family of three) and fall into the coverage gap with no affordable health insurance options.
-
- Another 158,000 uninsured Georgians make slightly above the poverty line (between 100 and 138 percent of poverty).[2]
- Most will qualify for premium subsidies on healthcare.gov, but they may not be able to use the coverage because of high deductibles or copayments. Medicaid does not have deductibles and has small copayments based on income.
- 1.4 million Georgians do not have health insurance, and Georgia’s uninsured rate of 13.7 percent is third highest in the country. In rural Georgia, the uninsured rate could climb to more than 25 percent by 2026.
- Closing the coverage gap can significantly strengthen mental health and addiction treatment and services in Georgia. About 25 percent of uninsured Georgians who would qualify for Medicaid expansion coverage suffer from mental illness or substance abuse.
Georgians need health coverage to stay healthy
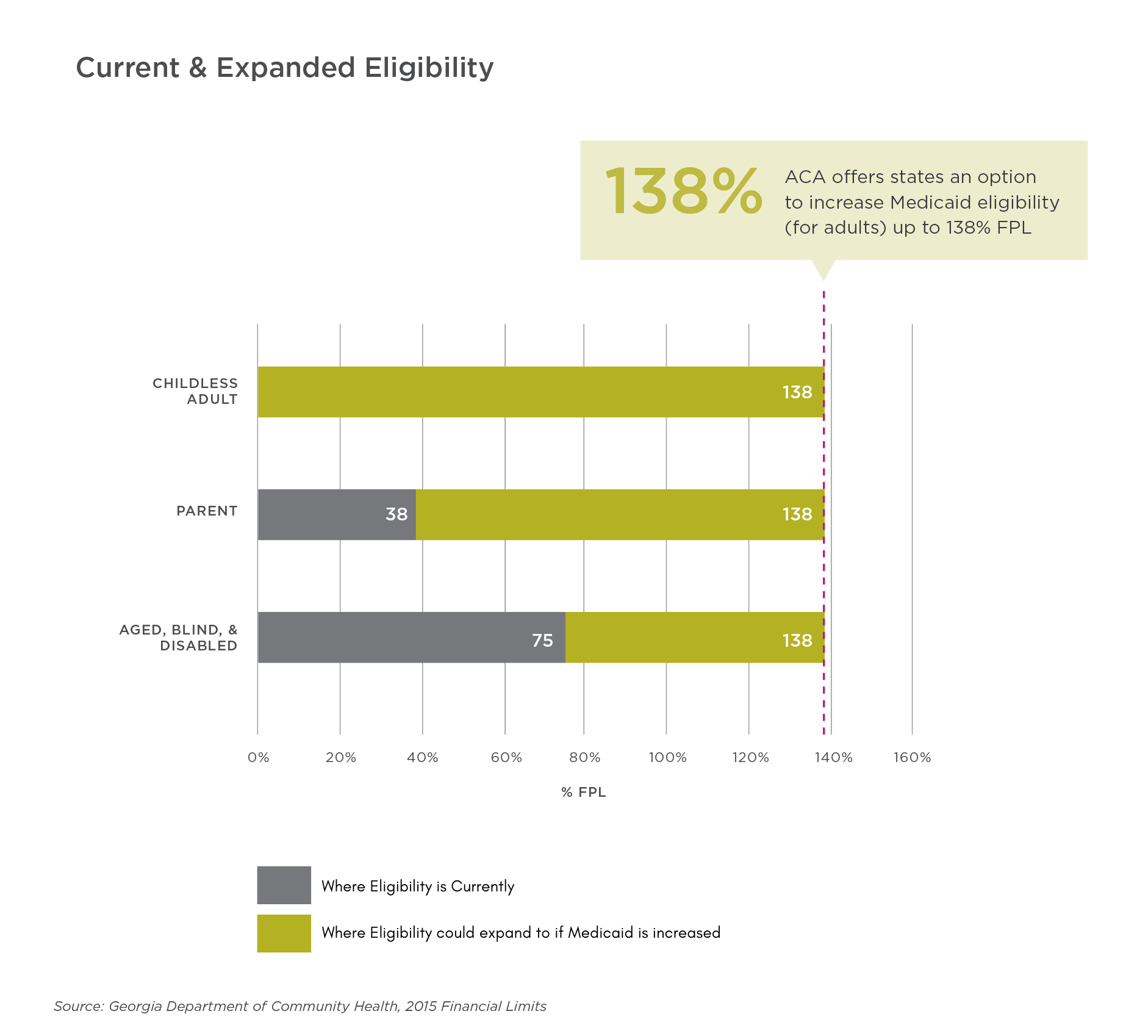
- Georgians who could gain coverage under Medicaid expansion earn below 138 percent of the federal poverty level, or about $14,580 for an individual, $19,720 for a family of two and $24,860 for a family of three.
- Sixty percent of people who would be covered by Medicaid expansion are working but often not offered health benefits through their job or do not get paid enough to afford their employer plan. Only 41 percent of Georgia employers offer employer-sponsored health insurance.
- Closing Georgia’s coverage gap would extend health insurance to over 155,000 uninsured women. Georgia ranks among the bottom five states for women’s health insurance coverage.
- Closing the coverage gap could extend health insurance to nearly half of Georgia’s uninsured veterans, expanding coverage to 32,000 uninsured veterans and military spouses in our state.
- Closing the coverage gap would help address racial disparities in health care access and outcomes. About 36 percent of Georgians in the coverage gap are Black, and 22 percent are Latinx.
Closing coverage gap yields economic benefits for state and helps accelerate economic recovery
- For every dollar the state spends on closing the coverage gap, Georgia receives up to $9 in federal funding.
- Closing the coverage gap could create 56,000 jobs in Georgia each year and boost the state’s economic output by $6.5 billion annually.
- Closing the coverage gap could create 12,000 jobs and $1.3 billion in new economic activity in Georgia’s rural communities each year.
- Georgians are already paying federal taxes toward closing our coverage gap, but state leaders have refused billions in federal health care dollars meant to pay for Georgians’ health coverage and stabilize struggling rural hospitals.
Improve Georgia's maternal health by expanding health coverage
- Review on Med. Ex's impact on reproductive & sexual health.
- 16% of Georgia women ages 15-49 (reproductive ages) are uninsured. (KFF)
- In recent Research America survey (slide #7), Georgians say substance use, mental health, and lack of insurance are top factors increasing risk of maternal mortality.
- Maternal mortality stats & disaggregated racial data from America's Health Rankings
- Maternal health outcomes in Georgia, by the Center for Reproductive Rights.
Stabilize struggling rural hospitals by closing the coverage gap
- Nine rural hospitals have shuttered since 2013 across the state, and more than half of Georgia’s remaining rural hospitals are financially vulnerable to closure. At least 118 counties in Georgia are considered rural because they have a population below 50,000.
- Many Georgia hospitals are struggling because they treat so many patients who lack health insurance and cannot afford high out-of-pocket costs. Closing the coverage gap opens up an important revenue stream to ensure rural communities have access to health care.
- Taxpayers end up paying a share of the cost for uninsured people who show up in emergency rooms. Closing the coverage gap would allow people to go to their doctor instead of the emergency room when they get sick.
- Other states see significant reductions in uncompensated care after closing their coverage gaps: Arkansas experienced a 56.4 percent decrease; Kentucky saw a 59.7 percent decrease.
Strengthen mental health, substance use treatment by expanding health coverage
- Closing the coverage gap can significantly strengthen behavioral health treatment and services in Georgia. About 25 percent of uninsured Georgians who would qualify for Medicaid expansion coverage suffer from mental illness or substance abuse.
- States that closed their coverage gap expanded treatment services to more people with mental illness or substance use disorders. Kentucky saw a 700 percent increase in Medicaid beneficiaries using substance use treatment services after the state expanded eligibility in 2014.
- Addiction is a disease and most people need treatment to get better. Good treatment works but many people don’t have the opportunity to get that treatment. We can support our friends, family and loved ones in the coverage gap by making sure they have access to Medicaid coverage and the addiction services they need.
- Access to Medicaid is particularly important for communities of color who, due to many barriers including socioeconomic factors, are less likely to have access to coverage, or complete treatment for substance use disorders than any other group.
- Opioid specific funding helps only the portion of individuals with opioid use disorders and leaves out the large numbers of people addicted to alcohol or other drugs. Providing Medicaid coverage improves access to treatment for people with all types of substance use disorders.
Georgia can afford to close the coverage gap
- Georgia can afford to close the coverage gap, but state leaders have so far chosen to spend tax dollars in other ways, like $309 million for insurance company tax breaks. State leaders could also increase Georgia’s extremely low tobacco tax to the national average to raise hundreds of millions of dollars a year. Three in four Georgians support raising the tobacco tax by $1, according to a recent poll.
- Closing the coverage gap would extend health coverage to almost half a million Georgians, support struggling hospitals, create 56,000 jobs and bring in $3 billion from the federal government. The annual net cost to Georgia would be $143 million in 2020.
Georgia can expand Medicaid in a few different ways
- The Georgia Department of Community Health, the state Medicaid agency, can submit a state plan amendment to the federal government. The federal government has 90 days to approve it. Most expansion states took this path, referred to as a “traditional” Medicaid expansion.
- The state Medicaid agency can submit a request to the federal government to waive certain parts of the Medicaid program. This plan, called an 1115 Medicaid waiver, can include increasing the Medicaid income eligibility to 138 percent of poverty (as intended by the Affordable Care Act). So far, seven states expanded Medicaid using waivers. For more about the differences between traditional Medicaid expansion and Medicaid 1115 waivers, see this fact sheet.
- In December of 2019, Georgia submitted an 1115 waiver that partially expanded Medicaid eligibility up to 100 percent of the poverty line. The plan has not yet been approved by federal officials, but it includes illegal work reporting requirements and is expected to only receive a 67 percent federal match instead of the full expansion’s 90 percent match. You can read more about Gov. Kemp’s Medicaid waiver plan here and here.
- Senate Bill (SB) 106, signed in March of 2019, restricted the Department of Community Health from extending coverage past the poverty line. State leaders should consider the following options to remove this restriction so more Georgians can receive Medicaid coverage:
-
- State lawmakers can amend SB 106 to allow expansion up to 138 percent of poverty and/or add language to the budget allowing the department to pursue a full expansion.
- The Governor should consider if his emergency powers would allow him to authorize a full Medicaid expansion by suspending the restrictions from SB 106 to prevent delay in pursuing expanded coverage. The governor’s public health emergency powers allow him to “suspend any regulatory statute prescribing the procedures for conduct of state business, or the orders, rules, or regulations of any state agency, if strict compliance with any statute, order, rule, or regulation would in any way prevent, hinder, or delay necessary action in coping with the emergency.”
- The Department of Community Health should consider ways to expand coverage through emergency 1115(a) Medicaid waivers and resubmitting the state’s current waiver to remove work reporting requirements and other provisions that impose barriers to coverage and care.
[1] Georgia Department of Community Health, July 8, 2019. Georgia Environmental Scan Report, Page17. “Count of Uninsured by Age & Poverty Status”
[2] See footnote 1
Download a pdf copy of this resource here.
Impacts of closing Georgia's coverage gap
- Impact 1: Closing the coverage gap can significantly strengthen behavioral health treatment and services in Georgia. About 25 percent of uninsured Georgians who would qualify for Medicaid expansion coverage suffer from mental illness or substance abuse.
- Impact 2: Opioid abuse and unmet mental health needs are decimating communities statewide, exacerbated by high uninsured rates among working Georgians who simply can’t afford access to care. States that closed their coverage gap expanded treatment services to more people with mental illness or substance use disorders.
- Impact 3: Closing Georgia’s coverage gap and expanding Medicaid would extend health insurance to more than 155,000 uninsured women in Georgia. Georgia ranks among the bottom five states for women’s health insurance coverage.
- Impact 4: Closing the coverage gap could extend health insurance to nearly half of Georgia’s uninsured veterans, expanding coverage to 32,000 uninsured veterans and military spouses in our state.