Blog
- Home
- >
- Cover Georgia Blog
- >
- After recent court decision,...
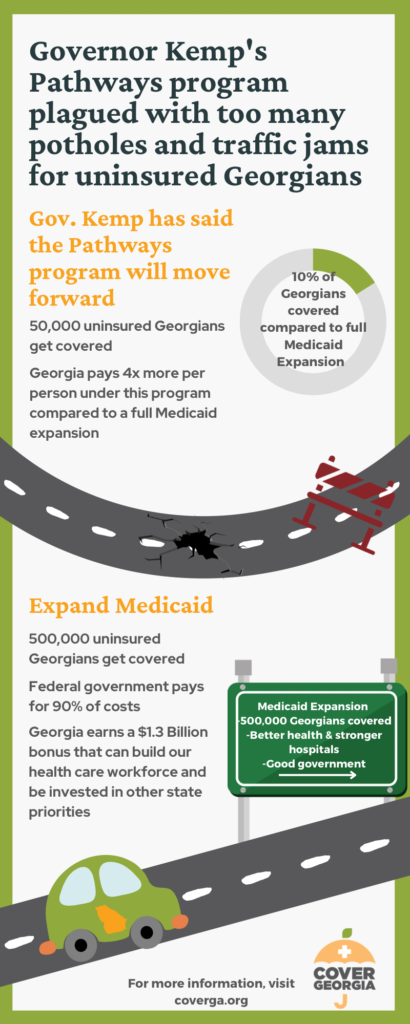
In 2019, Gov. Brian Kemp proposed a plan that would limit new Medicaid coverage to a much more restricted number of Georgians. The Governor’s plan would impose debunked “proof of work” requirements and require unaffordable premiums for some enrollees. The Trump administration approved the complete plan in 2020. In December 2021 the Biden administration changed its approval to disallow the burdensome work requirements and premiums. You can read more about the back-and-forth over the Governor’s plan in this blog and on our waiver timeline.
Background
In 2019, Georgia put forward a plan to expand Medicaid to a limited group of Georgians. Under the “Georgia Pathways” plan, the state would allow adults with incomes below the poverty line ($12,880 for an individual and $17,420 for a family of 2) to qualify for Medicaid health insurance. The Georgia Pathways plan also required these newly eligible adults to complete and document 80 hours of work (or other “qualifying activities”) each month to enroll in and keep their coverage. Some enrollees would also be required to pay a monthly premium to stay covered.
In 2020, the Trump administration approved the Pathways plan and implementation was set to begin in the summer of 2021. However, when the Biden Administration took over in the spring of 2021, they paused the approval to allow the new administration more time to review the Pathways plan. The Biden administration was particularly interested in the work requirements and premium payments and whether these additions violated the spirit and goals of the Medicaid program.
At the end of 2021, the Centers for Medicare and Medicaid Services (CMS) approved the Georgia Pathways plan, allowing Georgia to extend Medicaid coverage to Georgians making up to the poverty line (or 100% FPL). However, CMS denied the state’s request to include work requirements and premium payments as a condition of enrolling in and maintaining Medicaid coverage. CMS cited concerns about the devastating impact the COVID-19 pandemic has had on both the health and economic security of Georgians as the reason for denying these provisions. You can learn more about the Georgia Pathways program and the approval timeline here.
Recent Updates
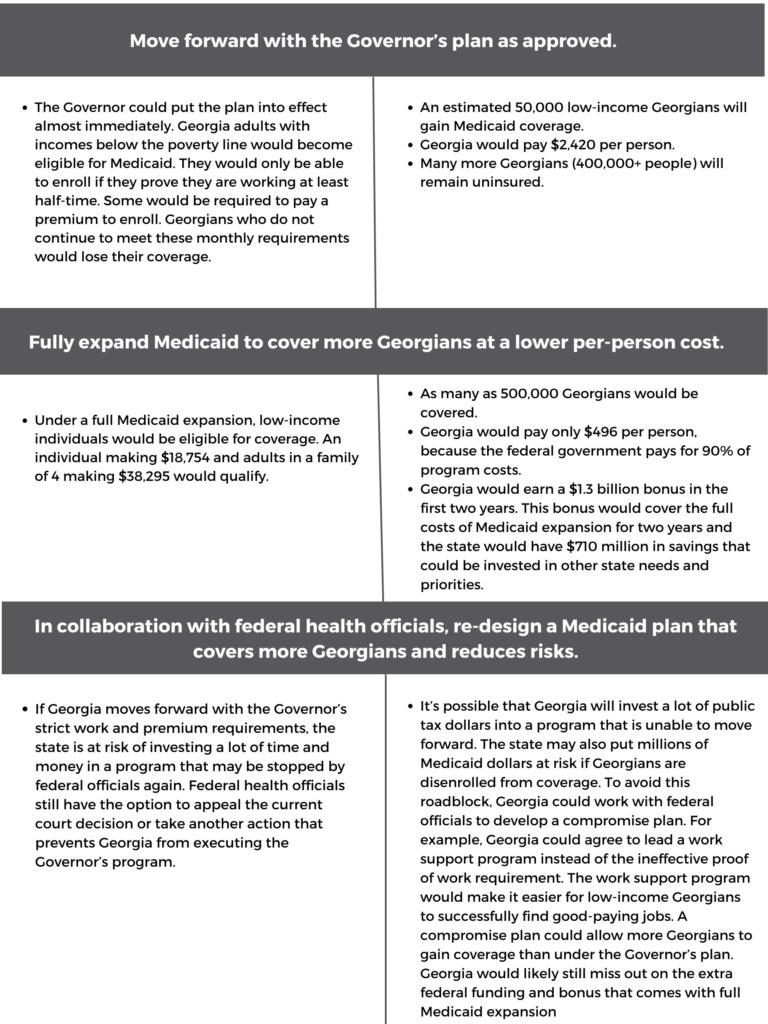
Following this final approval of the Pathway’s plan and denial of the request to include work requirements and premium payments, Governor Kemp was left with four options. He could do nothing and continue to let low-income Georgians remain uninsured, appeal CMS’s decision, implement the Pathways waiver without the work and premium requirements, or fully expand Medicaid to cover as many as 500,000 low-income Georgians (you can learn more about the options available following the waiver approval here). Governor Kemp chose the second option and appealed CMS’s decision to deny the inclusion of work requirements and premium payments.
In August 2022, a judge issued a ruling on the appeal of CMS’s decision. The judge ruled that the Biden Administration could not deny the previously approved work requirements and premium payments from the original Georgia Pathways plan. This decision means the state can move forward with implementation of the waiver as originally approved in 2020. CMS has yet to respond to this ruling, but does have the option to appeal the decision to a federal appeals court.
What does this court decision mean for Georgians?
Governor Kemp can carry out his Medicaid plan as he intended. If the program goes into effect, Georgia adults with incomes below the poverty line would become eligible for Medicaid. They would only be able to enroll if they complete monthly paperwork to prove they are working at least half-time. Some would also be required to pay premiums. Governor Kemp’s administration estimates that only about 50,000 Georgians (out of 500,000) would successfully gain coverage.
Most otherwise-eligible Georgians will be unable to enroll in or keep their Medicaid coverage because of the work requirements or premium payments.
The work requirements do not work for many uninsured Georgians. Georgians who are full-time caregivers, people in mental health & addiction recovery programs, and people living in areas where good jobs are harder to come by would not meet the work requirements. That means rural residents, people living in low-income communities, and communities of color are more likely to be left uninsured.
Georgia leaders can choose a better path
With this most recent court decision, Governor Kemp and the Georgia legislature once again face a choice about how to best connect low-income Georgians to health coverage and care.
Their options are:
Medicaid expansion is still the best option for Georgians
Full Medicaid expansion still makes the most sense for Georgia. Medicaid expansion would boost the health of Georgians by increasing early detection for diseases like cancer and heart disease. The expanded coverage would relieve the burden on rural hospitals, ensuring that their communities continue to have access to care. Medicaid expansion would close long-standing health gaps that unfairly cut short the lives of Black and brown Georgians.
Too many Georgians have been left without coverage for far too long. Our state leaders must choose the best way forward for our state. Medicaid expansion is the best way forward.